Change management in healthcare presents challenges you won’t find in many other industries.
In other industries, digital adoption is a no-brainer. Using digital tools to enhance and support your business lets you reap more profits and drive growth.
But when it comes to healthcare, it’s not that simple.
Why is that?
For one thing, digital transformation has a lower impact in healthcare. An analysis by McKinsey in 2020 revealed that only 35% of working hours in healthcare are automatable. The analysis concludes that by 203, an estimated 15% of healthcare working hours will be automated with the help of AI.
Those are paltry numbers compared to other industries.
On top of that, digital adoption in healthcare has a history of failure. In 2020, Forrester revealed that over the last decade, the adoption of electronic health records (EHRs) rose from under 20% to over 95%.
The U.S. Government invested billions of dollars to subsidize this digital transformation, believing it would boost clinician productivity.
It did not, and it turned out to be an expensive mistake that left clinicians with a bad taste in their mouths for digital adoption.
In this article, we’re shining a light on these mistakes to highlight the importance of change management in healthcare and to show that change is powerful and possible.
We will break down everything you need to know, from definitions to drivers and challenges to tips for success.
If you want to make a difference in the lives and experiences of clinicians and patients alike, you’ll find everything you need right here.
Change management in healthcare: Definition and importance
At its core, change management refers to the structured approach you take to transition individuals, teams, and organizations from a current state to a desired future state.
It’s all about understanding and managing how organizational changes affect those within it.
The importance of change management can’t be understated in the healthcare setting.
You’re dealing with an ever-evolving landscape, from technological innovations to policy changes. Effective change management ensures that these shifts occur smoothly and that your organization remains adaptive and resilient.
By embracing change management, you position your healthcare institution to weather challenges and capitalize on new opportunities.
4 Drivers for change management in healthcare
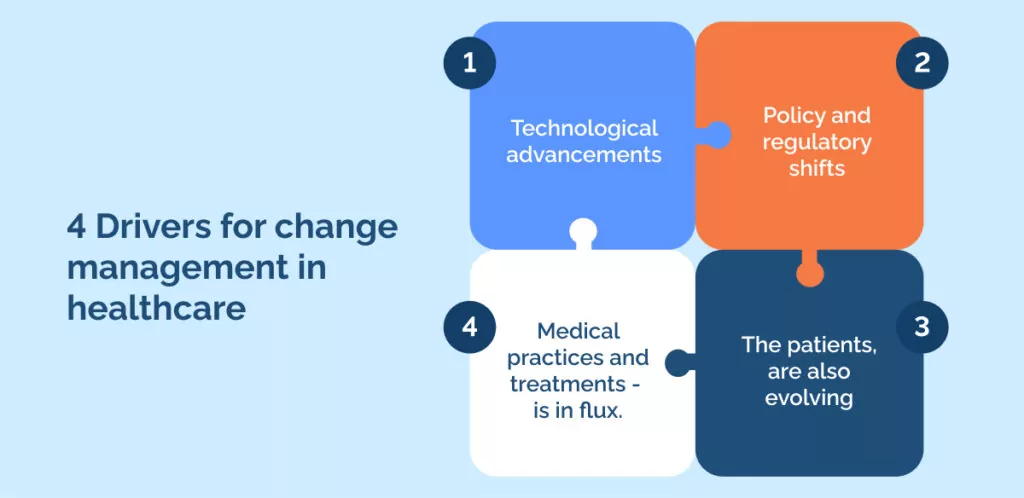
Many factors drive the need for change management in healthcare, but we think these 4 drivers rise to the surface as the most impactful and important.
Firstly, technological advancements play a pivotal role. From telemedicine to AI-powered diagnostic tools, emerging technologies can redefine how you deliver care, enhancing efficiency and patient outcomes.
Next, you must always be attuned to policy and regulatory shifts. Governments and regulatory bodies continually update guidelines and standards. Being proactive in response ensures that your organization remains compliant and ahead of the curve.
The people you serve, the patients, are also evolving. Their demographics change, and with them, their health needs and expectations. As the population ages or becomes more diverse, or as societal norms shift, the services and care they seek might differ from what was standard in the past.
Lastly, the heart of healthcare – medical practices and treatments – is in flux. New research, discoveries, and methodologies mean that what was considered best practice yesterday might not hold tomorrow. By staying updated, you ensure you always provide the best possible care.
Understanding these drivers ensures that you’re not just reacting to change but strategically planning for it.
4 Challenges in implementing change in healthcare
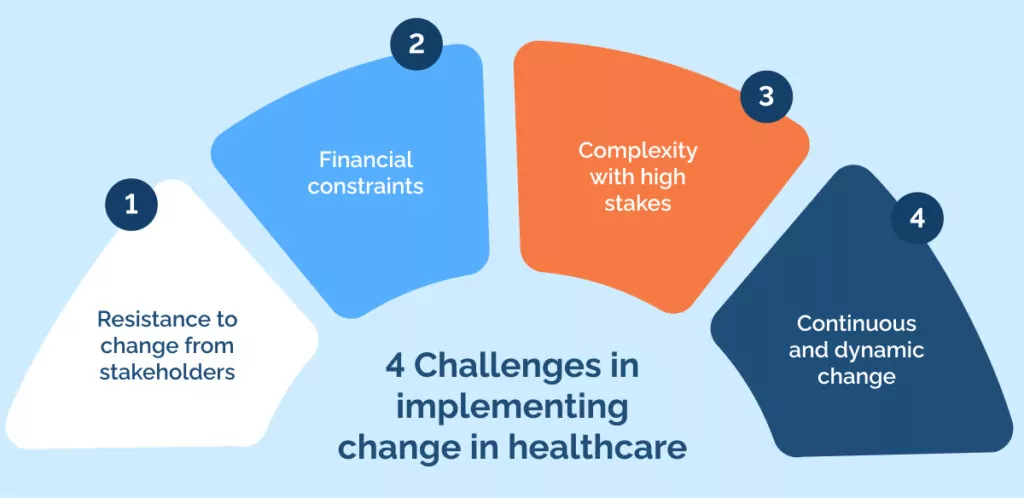
While recognizing the need for change in healthcare is one thing, implementing it presents its own challenges that you should be prepared to address.
Awareness of these challenges lets you strategize more effectively and ensures that the changes you implement lead to genuine improvements.
These 4 challenges should give you a good idea of what to expect:
1. Resistance to change from stakeholders
One of the first obstacles you might face is resistance from staff and stakeholders.
People often fear the unknown, and introducing changes can disrupt their comfort zones.
It’s essential to understand their concerns and provide reassurance, as getting their buy-in is crucial for the success of any change initiative.
2. Financial constraints
Financial constraints can also be a significant barrier.
Implementing new technologies, practices, or policies often comes with costs.
You need to find a balance between making necessary changes and staying within budgetary limits.
3. Complexity with high stakes
Another challenge lies in the inherent complexity of healthcare systems and processes.
Unlike other sectors, the stakes in healthcare are incredibly high. A minor oversight can have significant consequences.
Therefore, any changes made need to be thoroughly evaluated and meticulously implemented.
4. Continuous and dynamic change
Lastly, the dynamic nature of healthcare demands ongoing training and education.
Keeping your staff updated with the latest practices and technologies is a continuous task.
This not only requires resources but also the willingness of your team to learn and adapt.
5 Key principles of effective change management in healthcare
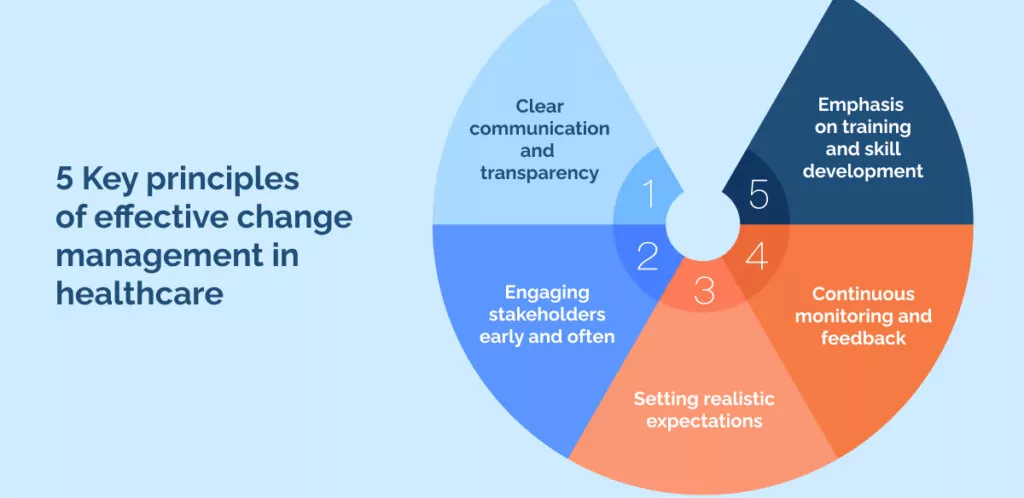
Change, especially in a sector as crucial as healthcare, demands a strategic and thoughtful approach.
To ensure that your change initiatives are both effective and accepted, we’ve compiled these 5 key principles of effective change management in healthcare.
By adhering to these principles, you’ll be better positioned to manage change effectively, ensuring your healthcare institution remains agile, adaptive, and ahead of the curve.
1. Clear communication and transparency
First and foremost, clear communication and transparency are vital.
When introducing change, it’s essential to communicate the reasons, benefits, and the process to everyone involved.
The more your team understands the “why” behind the change, the more likely they will support it.
2. Engaging stakeholders early and often
It’s also crucial to engage and involve stakeholders early in the process.
By seeking their insights and feedback, you tap into a wealth of experience and make them feel valued.
This involvement can significantly reduce resistance and foster a collaborative environment.
3. Setting realistic expectations
When rolling out changes, setting realistic expectations and timelines is key.
Remember, healthcare is complex, and rushing can lead to mistakes.
Giving yourself ample time and setting achievable milestones ensures the transition is smooth and effective.
4. Continuous monitoring and feedback
But the process doesn’t end once the change is implemented.
Continuous monitoring and feedback are essential to understand how the change affects your operations and the people involved.
Regular check-ins allow you to adjust as needed, ensuring the transition remains on track.
5. Emphasis on training and skill development
Lastly, place a strong emphasis on employee training.
Equip your team with the knowledge and skills to navigate the changes effectively.
This boosts their confidence and ensures that the change brings about the desired improvement.
Tools and techniques: Kotter’s 8-step change model
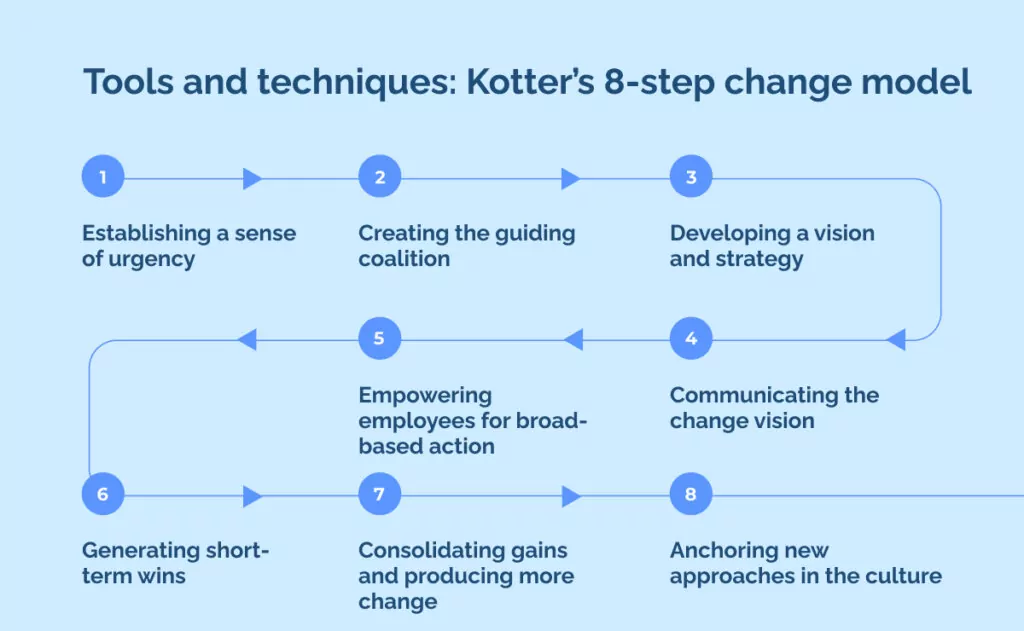
There are many different tools and techniques you could use to streamline your change management, and there’s definitely no one right answer to which tool is best, but you should definitely use something.
By following established change theory, you streamline the change process, ensuring that every step is grounded in a proven methodology tailored to the unique needs of healthcare.
If you’re looking for a good place to start, consider Kotter’s 8-step change model.
Kotter’s 8-Step Change Model is a robust approach to implementing change successfully. In the healthcare setting, it offers a structured way to drive transformations effectively, ensuring alignment with goals and reducing resistance.
Let’s delve into how each step aligns with common tools and techniques used in the healthcare change process.
Step 1: Establishing a sense of urgency
Before initiating any change, gauge the current atmosphere.
Understand where the organization stands and the level of perceived urgency.
This helps you identify potential challenges and tailor your approach.
Step 2: Creating the guiding coalition
Identify key players and influencers within the organization.
These individuals will be pivotal in driving change and garnering support.
Step 3: Developing a vision and strategy
A clear vision serves as a guiding light for the change process.
Ensure you have a comprehensive communication plan to articulate this vision effectively across all levels.
Step 4: Communicating the change vision
Repeatedly share the vision and associated benefits.
This will not only foster understanding but also build excitement and buy-in.
Step 5: Empowering employees for broad-based action
Equip your team with the necessary skills and knowledge to be active participants in the change process.
Continuous training ensures they feel confident and capable.
Step 6: Generating short-term wins
Celebrate small victories along the way.
Regular feedback sessions can help identify these wins and keep morale high.
Step 7: Consolidating gains and producing more change
Continuous improvement is key.
Use feedback to understand areas that still need attention and drive further changes based on insights.
Step 8: Anchoring new approaches in the culture
Ensure that the new methodologies and practices become integral to the organizational culture.
Regular training and reiteration can help embed these changes deeply.
Healthcare & change management: An outlook on the future

To anticipate the future, we’ll look to the recent past.
Here are a few of the things that change managers in healthcare organizations need to keep in mind.
The aftermath of the pandemic has reshaped many aspects of healthcare, from patient behavior to operational practices.
You’ll find that some changes are temporary, while others are here to stay. Adapting to this new normal means being proactive, understanding the long-term impacts of the pandemic, and strategizing accordingly.
The digital wave has been sweeping across industries, and healthcare is no exception.
Innovations such as artificial intelligence (AI), telemedicine, and digital health platforms are not just trends but necessities.
As technology evolves, you should be prepared to leverage it to improve patient care, optimize operations, and stay competitive.
While some changes can be anticipated, the nature of the healthcare industry means that unpredictability is part of the game.
Whether it’s a sudden regulatory shift, a new disease outbreak, or a groundbreaking medical discovery, you must cultivate an agile mindset.
Building a flexible and adaptive organizational structure ensures you’re always ready to pivot and respond to the unknown.
Tristan Ovington
Tristan Ovington is a professional senior writer and journalist, specializing in providing expert insights on various topics such as digital adoption, digital transformation, change management, and Cloud apps. He delivers his knowledge through accessible online content that is data-driven and presented in a friendly tone, making it easy for readers to understand and implement.